The big picture – ‘Tuning’ the Emergency Department engine
 Stepping back from the practicalities of the ED and Urgent Care Centre trials it is good to consider the big picture and what we are trying to achieve.
Stepping back from the practicalities of the ED and Urgent Care Centre trials it is good to consider the big picture and what we are trying to achieve.
As with any engine, significant improvements in performance can be achieved by multiple changes, even minor ones. It’s the same principle used to tune Formula 1 cars, sadly without the same resources!
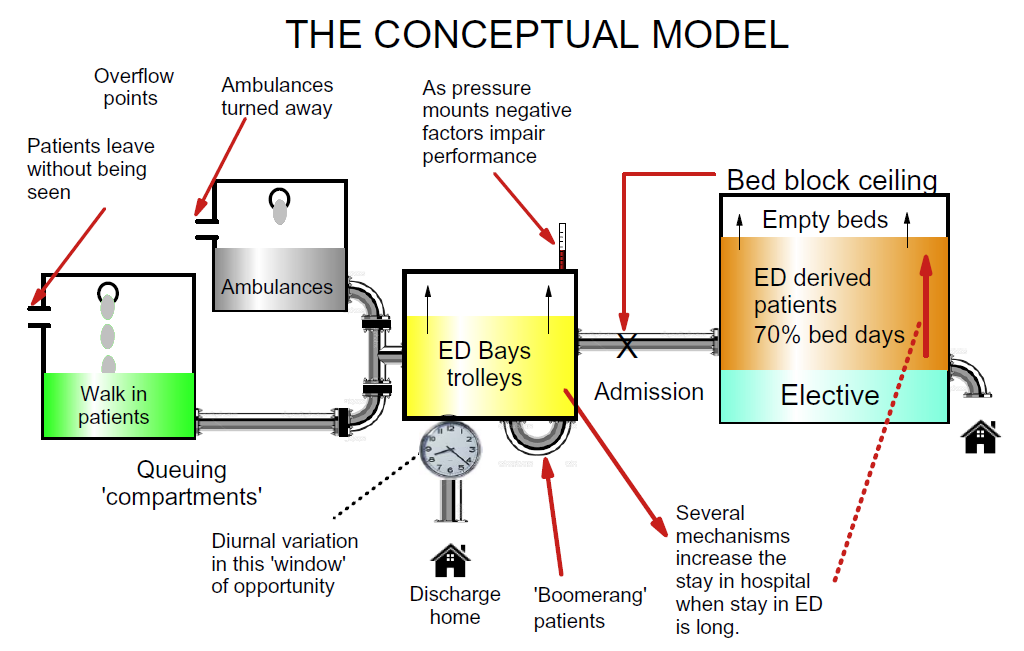
Our starting point was building a comprehensive model of the system. A simplified version is shown below. The ED and UCC are key ‘inlets’ controlling the flow of ambulance and walk in patients into the ED. Outflow is dependent on discharge home or admission. Thus we also need to consider the hospital ‘compartment’ where bed block can prevent admission from ED.
Discharging patients home is more difficult in the small hours, particularly for patients who live alone, thus there is diurnal variation in both departures and arrivals.
Repositioning In the first ED trial we explored whether repositioning two key events (ordering of investigations and treatments) could be achieved. These events in the standard ICHT process occurred respectively at median times 50 minutes and 80 minutes after arrival. SortED results showed the same investigations could be identified within minutes of assessing the patient.
Pitstop versus serial processing The ED trial results showed that serial processing is still evident despite some elements of RAT being introduced at ICHT. This makes at least some contribution to 4-hour breaches. Dividing the patients into quartiles for time of investigation, those with investigations ordered in the lower quartile (under 18 minutes from arrival) had 25/96 26% breaches. Those with investigations in the upper quartile, over 76 minutes from arrival, had 47/100 47% percent breaches, with the intervening quartiles 29% and 36.2% breached respectively. SortED can shift the ordering of investigations to the initial assessment < 10 minutes after arrival.
Disposition & PlacED™ Disposition is the process of directing each patient to the right area, deploying the available facilities to best effect. In our ED trial we focussed on choosing the best location within the department (Resus. area, Majors, Minors etc.) or ancillary facilities such as the Ambulatory Emergency Care (AEC) unit and UCC. In the case of the UCC we are examining whether we can use SortED as an aid to streaming, increasing the within-UCC options (‘see & treat’, see GP or nurse in UCC) and reducing the tendency to send the patient round to the ED.
Information gathering In both ED and UCC, SortED aims to improve the efficiency and clinical relevance of information gathered at initial assessment. Hand-written or typed triage/streaming notes are not an efficient method for the onward transmission of information to other clinicians. Nurses using SortED typed less, but gathered more clinically relevant information than either triage nurses or GP streamers: more face-time with the patient, less time at a keyboard.
With an eye to the future, pattern-recognition applied to SortED data should have potential for next-generation SortED devices.
Queuing The walk in and ambulance patient queues impose characteristic behaviour on Emergency Departments. Surprisingly, ED overload can be predicted and Mark Leaning is working on that area.
Gillie Francis – Dec 2017


